The Palliative Care Policy GPS
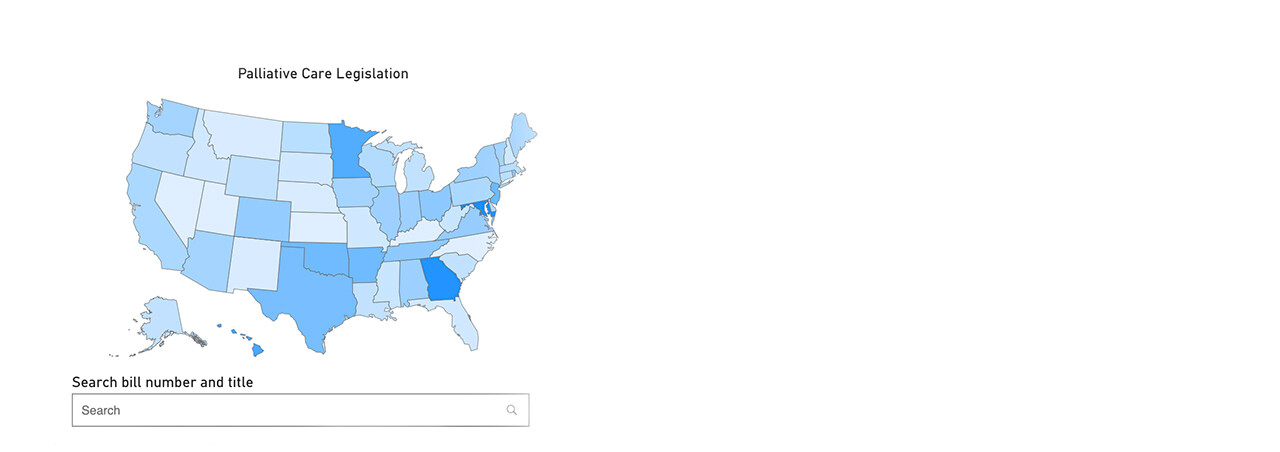
The Solomon Center for Health Law and Policy and the Center to Advance Palliative Care (CAPC) have launched an innovative new initiative — the Palliative Care Policy GPS (GPS) — a publicly accessible and regularly updated database that tracks state policies on palliative care and related services.
Visit the Palliative Care Law and Policy GPS Website
In recent years, state policymakers have increasingly paid more attention to palliative care, improving access and quality along the way. The importance of palliative care, which focuses on providing relief from symptoms and stress of serious illness to improve quality of life, and the need for innovative policymaking to support it, has become clearer over the past year and a half. But tracking developments in policies and regulations across states has been difficult. States maintain their own data on legislation and regulations, with no centralized platform bringing together information from across the country.
The GPS aims to fill this gap. It tracks policies related to palliative care across the 50 states, Washington, D.C., the Indian Health Service (IHS), the Department of Veterans Affairs (VA), and U.S. territories. By consolidating the landscape of state policymaking, the GPS offers a new tool for health care professionals, policymakers, palliative care champions, payers, and purchasers to search, compare, gain new ideas, and stay up-to-date on policy developments. The GPS has three primary aims:
- to provide a detailed and continuously updated database tracking palliative care policies
- to support cutting-edge research, including by students, on palliative care policy drawing on the information gathered
- to encourage policy innovation aimed at ameliorating disparities in access and quality.
The GPS will serve as a resource for palliative care advocates working with their own state policymakers to craft more effective laws bolstering the field. The GPS classifies palliative care legislation in seven core categories: workforce, payment, quality/standards, clinical skill-building, pediatric palliative care, public awareness, and telehealth. Legislation can be sorted by location, category, status, and timeframe. Users can assess legislative developments over time all in one place, encouraging the identification of trends, gaps, innovative policy initiatives, and best practices. These advancements could ameliorate disparities in access to high-quality palliative care, expand the palliative care workforce, drive essential skills across key clinicians, and increase public awareness of palliative care
Building a Coalition of Palliative Care Advocates
The GPS represents a unique partnership between a community of students and experts at Yale and beyond. The GPS marks a first-of-its-kind collaboration with CAPC, a national organization dedicated to increasing the availability of quality health care for people living with a serious illness. CAPC is part of the Icahn School of Medicine at Mount Sinai, in New York City.
Yale Law School students have been centrally involved in the process of creating and maintaining the GPS. Over the 2020–2021 academic year, students provided vital contributions — ranging from conducting the initial surveys of all 50 states and related entities to successfully submitting articles and abstracts on the GPS and researching bills addressing palliative care across the country.
Scholarly collaboration has been essential in fostering the Solomon Center's palliative care initiatives. In fall 2020, the Solomon Center convened a working group comprising palliative care scholars, practitioners, and advocates from a variety of institutions. In addition to providing invaluable advice on the function and future of the GPS, the working group supports a range of research and writing from cutting-edge studies on palliative care to work that will translate findings into targeted policy recommendations.