Solomon Center and CAPC Launch Innovative Palliative Care Policy-Tracking Database

In recent years, state policymakers have increasingly paid more attention to palliative care, improving access and quality along the way. The importance of palliative care, which focuses on providing relief from symptoms and stress of serious illness to improve quality of life, and the need for innovative policymaking to support it, has become clearer over the past year and a half. The COVID-19 pandemic increased the demand for palliative care and exacerbated many of the challenges it addresses, straining hospitals and communities across the country. But tracking developments in policies and regulations across states has been difficult. States maintain their own data on legislation and regulations, with no centralized platform bringing together information from across the country.
The Solomon Center for Health Law and Policy4 and the Center to Advance Palliative Care (CAPC)5 aim to fill the gap with an innovative new initiative — the Palliative Care Policy GPS6 (GPS) — a publicly accessible and regularly updated database that tracks state policies on palliative care and related services.
“The new Palliative Care Policy GPS is an invaluable tool to help us understand the policy trends and impact, and create a foundation for more evidence-based policy-making in the future,” said Stacie Sinclair, Associate Director for Policy at CAPC.
The GPS tracks policies related to palliative care across the 50 states, Washington, D.C., the Indian Health Service (IHS), the Department of Veterans Affairs (VA), and U.S. territories. By consolidating the landscape of state policymaking, the GPS offers a new tool for health care professionals, policymakers, palliative care champions, payers, and purchasers to search, compare, gain new ideas, and stay up-to-date on policy developments. The GPS has three primary aims:
- to provide a detailed and continuously updated database tracking palliative care policies
- to support cutting-edge research, including by students, on palliative care policy drawing on the information gathered
- to encourage policy innovation aimed at ameliorating disparities in access and quality.
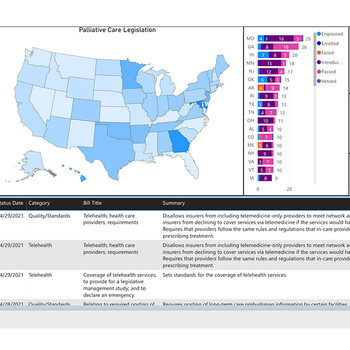
The GPS will serve as a resource for palliative care advocates working with their own state policymakers to craft more effective laws bolstering the field. The GPS classifies palliative care legislation in seven core categories: workforce, payment, quality/standards, clinical skill building, pediatric palliative care, public awareness and telehealth. Legislation can be sorted by location, category, status, and timeframe. Users can assess legislative developments over time all in one place, encouraging the identification of trends, gaps, innovative policy initiatives, and best practices. These advancements could ameliorate disparities in access to high-quality palliative care, expand the palliative care workforce, drive essential skills across key clinicians, and increase public awareness of palliative care, according to those involved in the project.
The GPS represents a unique collaboration between a community of students and experts at Yale and beyond.
“The Palliative Care Policy GPS would not have been possible without many key collaborators, including our partners at the Center to Advance Palliative Care, the members of our Palliative Care GPS Working Group, Yale University’s web development experts, and an outstanding student research team,” said Eugene Rusyn ’17, Editor-in-Chief of the Palliative Care Policy GPS, and former Senior Research Fellow and Lecturer in Law at Yale Law School.
Yale Law School students have been centrally involved in the process of creating and maintaining the GPS. Over the 2020–2021 academic year, students provided vital contributions — ranging from conducting the initial surveys of all 50 states and related entities to successfully submitting articles and abstracts on the GPS and researching bills addressing palliative care across the country.
“The experience gave me a glimpse into the legislative workings of different states,” said Stephanie Rice ’23, who worked on the project. “Some had constructed sophisticated programs to support the delivery of palliative care, while others had no legislation for it at all. After learning firsthand how much time it takes to track down this information, I’m glad my work has helped create a centralized location where people can learn about state palliative care policies in one place.”
This project marks the most recent expansion of the Solomon Center’s palliative care initiative7. It joins the Palliative Medical Legal Partnership, the Palliative Care Working Group, and the Elder Law Project. In fall 2020, the Solomon Center convened a working group comprising palliative care scholars, practitioners, and advocates from a variety of institutions. In addition to providing invaluable advice on the function and future of the GPS, the working group supports a range of research and writing from cutting-edge studies on palliative care to work that will translate findings into targeted policy recommendations.
“There is a great need for palliative care research to increase the evidence base for the field and subsequently improve care for patients and families facing serious illness,” said Dena Shulman-Green, Associate Professor at the New York University Rory Meyers College of Nursing and a member of the working group. “The Palliative Care GPS serves as a real-time clearinghouse for information on state palliative care policy that will enable research related to palliative care legislation and inform policy development.”
In coming months, the GPS will expand to include state regulations and federal legislation. The database will also be utilized to address innovative research questions and develop tools to support effective advocacy. Throughout, the GPS will highlight the power of state-level policymaking — the database already contains hundreds of bills, reflecting robust activity across states. It will also highlight a commitment to ensuring that the IHS, the VA, and the territories are included in the national policy dialogue. Taken together, the GPS aims to empower users and encourage policy innovation during a transformative time for palliative care.
The Center to Advance Palliative Care (CAPC)5 is a national organization dedicated to increasing the availability of quality health care for people living with a serious illness. As the nation’s leading resource in its field, CAPC provides health care professionals and organizations with the training, tools, and technical assistance necessary to effectively meet this need.
The Solomon Center for Health Law and Policy at Yale Law School4 is the first of its kind to focus on the intersection of law and the governance, practice, and business of health care. The Center brings together leading experts and practitioners from the public and private sectors to address cutting-edge questions of health law and policy, and to train the next generation of top health lawyers, industry leaders, policymakers, and academics.


